 Sebo Marketing
Sebo Marketing
 October 18th, 2021
October 18th, 2021
Without a doubt, this is one of the most controversial areas in orthodontics today. There are many vocal proponents on both sides of the discussion. It is clear that it would, in many ways, be simpler for the orthodontic profession if it was shown that there was no relationship, but I believe that upon examining the evidence that this relationship will be indisputable. The problem is not really the biology or the lack of statistical analysis or scientific dentistry. The problem is in the language we use and the lack of definition of terms. In fact, much of the time, we are rarely effectively communicating with each other.
Part I of this series is devoted to exploring the anatomy and pathology of the T M Joint and part II will be devoted to what the dentist providing orthodontic care needs to do in treating their patients.
When we speak about TMD, we are referring to disorders in the T M Joint. Medicine has a specialty in orthopedic medicine which has as its focus the bones and joints. Dentistry has never established a separate branch to deal with its foundational joint, so it makes sense to reach out to our medical colleagues in orthopedics for some insight. The very first problem you will see is that we have is that we do not use terms appropriately.
If you had a lot of pain in your arm, about half way between the wrist and shoulder when you tried to bend your arm, you might consult with an orthopedic physician. Imagine how you would react if after a thoughtful examination, he proclaimed that you had “elbow” and suggested a course of treatment that included anti inflammatory drugs, mobilization and warm compresses based on that diagnosis. What if you went to see another orthopedic physician who also diagnosed you with “elbow”, but instead recommended a course of treatment that involved surgery of the elbow and then immobilization with a cast? Most half way intelligent patients would run for the door.
The problem is that elbow is the name of a joint, not a disease. Many diseases could affect that specific joint. In the case of our patient, they might have had a fracture in the ulna bone below the humerus. A fracture would require immobilization and perhaps even a surgically inserted pin for stabilization. (1)
Mobilization would be the very worst thing that could be recommended. Or they might have had bursitis in the joint. This is an inflammatory process that requires anti-inflammatory drugs and mobilization to insure that full range of motion is regained. (2)
Or there might have been a ganglion cyst of the elbow. When conservative treatment fails, surgical excision of the cyst is recommended, through an open or arthroscopic approach. (3) Another possibility might be Rheumatoid arthritis in the elbow. (4) All of these are diseases of the elbow, all are different and all require different treatment. Diagnosis always precedes treatment for any condition.
Another important consideration is to understand how diseases evolve from some vague set of symptoms to a mature and well understood disease. In the beginning most start out as a signs and symptoms. Some practitioners begin to notice associations and a syndrome is born. At that point causality in not understood, terminology is vague and inconsistent, there is much disagreement among professionals and treatments are mostly symptomatic and results are inconsistent. Over time as more is observed, the disease becomes better understood, terminology is clarified and matures to the point that most practitioners can accurately identify the disease and treatment methodologies come into agreement. Such is the case with diseases of the elbow joint.
The other very important requirement is that we are able to separate structural damage from pain. Some people can have pain and a structural deformity cannot be identified. A patient can have pain in an area that is due to reversible inflammation or over use in the case of muscles with no measurable structural damage. Or a patient can have structural damage, such as a dislocated disc in a joint that may not cause pain. Going back to medicine, it is agreed that many people have herniated discs in their spine and some of them have pain and others are asymptomatic with the same radiographic presentation. (5) We cannot even assume that a patient who presents with pain and has a structural deformity has a cause and effect relationship between the two. And further we must refer back to the work of Travell (6) and others to understand the concept of referred pain so we do not rely on the reports of the patient for the full diagnosis.
In dentistry the diagnosis of “TMD” is offered to patients every day and then various treatments are suggested. Every one aggress that some treatments seem to work at least some of the time, some do not and sometimes the “problem” seems to go away by itself, so perhaps no treatment was needed. If our medical orthopedic colleagues approached every elbow problem the way most dentists seem to approach T M Joint disease, I can imagine that they would have about the same degree of success that we do and at least as much controversy in the field. By now I think that it should be pretty clear that our problem in dentistry is that we have skipped the all important step of specific diagnosis of the problem.
We need to take some steps back and understand that we are dealing with an orthopedic issue that requires a diagnosis first. What is the specific problem in the area and then second, what can be done to alleviate it? If we miss the diagnosis and apply the incorrect treatment, regardless how carefully it is executed, we will not have success. If we diagnose correctly and apply the correct treatment, but do not execute it to the necessary standards, the results will be equally ineffective. And of course if we diagnose correctly and apply the correct treatment, but do not execute it completely, the results will be equally unsatisfactory.
In the case of TMD, there are in fact many specific maladies that could affect the area. That includes diseases in the bones of the joint, the soft tissues in the joint such as the ligaments and disc and the primary muscles that are attached to the mandible and the skull.
The joint itself is a ball and socket joint that is load bearing. It is most stable as the condyle (ball) is allowed to center in the glenoid fossa (socket). (Fig 1) There is a tower of muscles from the cranium down to the breast bones that suspends two floating bones, the mandible and hyoid bone. (Fig 2) In order to execute the life essential reflex of swallowing this whole complex must be stabilized. In order for that to happen, the teeth must be brought together into an intercuspated position of relative stability to support the mandible which in turn supports the hyoid bone so that the tongue and related muscles can execute the swallowing reflex. As a consequence of this required positioning, in many people, the mandible must be distracted out of the centered and inherently more stable position in the center of the fossa. This potentially unstable position that is required for swallowing must be maintained by heightened and prolonged muscle activity as opposed to simple stabilization by ligaments. In addition, some people are stimulated to clench or grind their teeth as a result of this conflict between the centered position of the jaw joint and the maximally intercuspated position of the teeth. (7)
For purposes of organization, I divide the TMD problems into 3 categories. First, there are those that affect the teeth and supporting structures, primarily the teeth, periodontium and supporting alveolar structures. Second, those that affects the joint itself including the disc, cartilage and bone. And third, those that affect the related structures outside the actual joint, primarily the muscles of the T M Joint. Each of those areas can have structural damage that is observable and measurable. And each of those areas can have pain issues that are reportable, but sometimes measurable and sometimes not.
As an example, it is not uncommon to see a patient with a displaced disc that clicks on opening and closing but does not have pain. Do they require treatment? What about a patient that has no history of joint sounds, but does have pain. Do they require treatment and if so what treatment? What about a patient that has significant wear of their teeth and has evidence of clenching and grinding their teeth, but has no pain and no joint sounds, do they require treatment? And what about a patient with advanced periodontal disease and alveolar bone loss in the posterior segments, do they require bite treatment?
Let’s look at these one at a time, although there are certainly cases where one patient has multiple simultaneous issues.
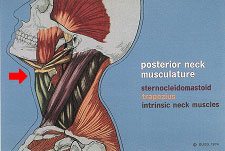
Fig 2. Drawing of the muscles from the skull to the shoulders and chest.
Dentists for over 100 years have applied the laws of elementary physics to the jaw and teeth. The fulcrum is in the T M Joint and the force is in the muscles and the resultant is in the teeth. Although the T M Joint is a complicated system, in many respects it is a class III lever. Force is greatest closest to the joint. The teeth themselves are also subject to the laws of physics as well in that vertical forces are much better resisted than lateral forces. (Fig. 3) Certainly any engineer or orthopedic surgeon would agree that it is imperative to design a biologic system to minimize stress so the forces would be directed in the long axis of the support and placed as far from the fulcrum as practical. Clearly the patient in Fig. 4 and 5 has damaged teeth that have been caused by tooth grinding and clenching. Further there is much support in the literature for an uneven bite being a trigger for teeth clenching and grinding. (8,9,10,11,12,13,14,15)
Fig 3. Drawing of the forces of occlusion applied to teeth.

Fig 4. Worn and broken teeth.

Fig 5. Match up proves grinding.
This subject is far to complex to cover fully here but suffice it to say that disease in the joint can be in the soft structures of the disc and ligaments or could be in the hard structures of the bone or cartilage. The diagnosis of joint disease requires both a clinical examination as well as imaging with MRI and CAT scans to get a full evaluation. (16) The clicking and popping sounds of the T M Joint are due to the fact that the ligaments have been damaged allowing the muscles, particularly the lateral pterygoid to pull the disc out of the bracing position between the condyle and the socket. In Fig. 6 & 7 you can see that the disc is displaced in the centered jaw position but in protrusive the condyle moves under the disc creating the classic click or pop sounds. The conventional thinking that joint sounds are signs of damage and lack of joint sounds is a sign of no damage in the joint is completely wrong. (Fig. 8,9) In fact, joints that used to click and have stopped clicking are in fact worse and these joints are more likely to result in long term osseous damage. (17) In addition tooth clenching and grinding has been shown to be associated with damage to the joint due to the compressive loads that are placed on the joint (18)

Fig 6. MRI of the jaw in centered position shows the disc is anteriorly distracted from the centered portion of the joint.

Fig 7. MRI of the jaw in protrusive shows the disc is recaptured when the condyle moves forward. As a result there is a click.

Fig 8. MRI of the jaw in centered shows the disc is anteriorly distracted from the centered portion of the joint.

Fig 8. MRI of the jaw in centered shows the disc is anteriorly distracted from the centered portion of the joint.
Many patients get significant head, neck and facial pain. (19,20,21) In clinical practice the most common presenting pain symptoms we see are patients presenting with pain in the face, jaws and head that is due to muscles. The medical literature reports that muscles have a significant affect in pain in the head and neck. (22, 23, 24) Of course there are many causes of head, neck and facial pain that do not relate to the T M Joint or muscles or occlusion and that is why diagnosis is the key to success.
This muscle pain is often due to over use of the muscles that is due to clenching and grinding the teeth that can lead to over use of the muscles and pain. This source of pain while very common and the cause of significant disability in the population can be difficult to diagnose because there are no objective tests such as radiographs or blood tests to confirm the diagnosis. As a consequence of this, many patients who suffer from head, neck and facial pain are unhappy with their treatment. (25)
There are multiple conditions and disease states than can relate to the T M Joint. (26,27,28,29) If there is damage or dysfunction is the teeth or supporting structures, or damage or pain in the joint, or pain in the muscles and the occlusion is indeed a factor, treatment is needed. The next article will be devoted to what the dentist providing orthodontic treatment needs to know and do to detect T M Joint disorders before treatment and what to do during treatment to minimize the future potential T M Joint disorders.
